Ignatius the tenacious
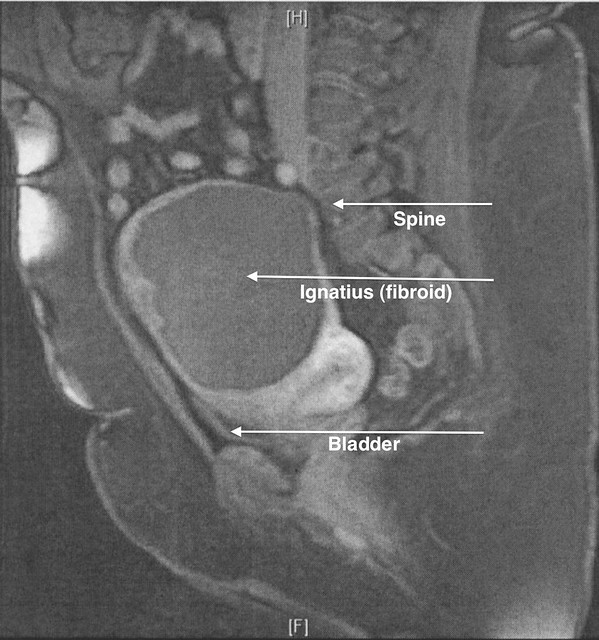
In this episode of General Hospital, on Tuesday the 16th, the day after my annual physical, I set off for Northwestern Memorial Hospital to consult Dr. M. about performing a laparoscopic myomectomy on the remains of Ignatius, the tenacious fibroid that, eight months after an 18 August 2008 uterine fibroid embolization (UFE), had shrunk no more than 1 centimeter. As you can see in the MRI image, Ignatius still takes up more space than some vital organs. My back and legs hurt, I feel bloated, and my bladder capacity seems to be less than a cup of coffee, let alone a mug. It has to go, and I was hoping that Dr. M. would be willing to take this project on, despite its size and mine.
I didn’t complete any paperwork, so after introducing himself and sitting me down, Dr. M. asked the status and health questions you’d expect from a gynecologist, including the name of my current gynecologist (“Oh, she’s very good.”). One question threw me off, however: “Are you in a relationship? That seemed awfully personal. What happened to the traditional, tried-and-true “Are you single, married, divorced, or widowed?”? I supposed “partnered” (if awkward in construction) could be added to cover every base, but “Are you in a relationship?” sounded like something I’d expect from a therapist or match.com.
I answered with a simple “no.” But the things I wanted to say . . .
He asked me the question every specialist who’s new to me asks: “Why are you here?” I find this disconcerting because in most cases, including this one, they know why — they have a referral. Sometimes I feel like it’s a test to see if I can describe my condition accurately enough to eliminate the possibility of hypochondria. I told him what I knew, about how long I’d known it, how the UFE had proven to be ineffective, and that I’d been told he may be able to perform a laparoscopic myomectomy. “I think you have the images.” Indeed, he did. I thought so.
He’d asked me if I’d considered a hysterectomy, and I said “no” in a tone that I hoped conveyed resolve. He warned me that the myomectomy could turn into a hysterectomy (I’d received the same warning about the UFE), but quickly added, “But I’ve never had to do that.” Later I noticed he’d written “NO hysterectomy” in his notes, too.
Dr. M. noted a couple of risk factors, neither of which, to my surprise, was my weight. The first was the long appendectomy scar on the right side of my abdomen that runs from a little below the level of my navel to the level of my pubic bone. The other is the degenerated nature of Ignatius, which is no longer solid muscle tissue but more of a cream cheese consistency, as he put it. It might take two hours, he said, then corrected himself to three, presumably because of its size and consistency. I brought up the size again, and he said that not many besides him would do this on me. I’m not sure I found that as reassuring as it was intended to be, but at least he said the uterine wall is in good shape.
On the way to the examining room, where he wanted to see my scar, I told him that my fibroid is named Ignatius. He asked if I call it “Iggie” or any other nickname, but I said we try to keep a more formal relationship (appropriate, I think, when one party has killed and is now trying to excise the other). He rattled off some of the other names he’d heard from other patients, although I don’t remember them. When I mentioned that I would have liked to have had the pre-UFE Ignatius in a jar, he offered to take photos. I liked this in him — he allows a certain sense of humor and humanity to show, unlike many physicians. He didn’t correct anything I said or explain anything that I already knew, so I felt like I was being treated like an intelligent and informed patient — whatever the actual case may be.
The appendectomy scar, it appears, is far enough over that it shouldn’t be a factor. He marked the likely incision points (I’ve forgotten how many — six?), none of which is very close to the scar. They seemed to form a circle around my navel. This should look interesting afterward! He asked if the scar bothers me, and I said no (while it’s a little more sensitive to touch and used to “pull” a little once in a while, for the most part I don’t notice it except for its ghastly appearance). If it bothers me, he said, he could have a plastic surgeon take care of it. The offer was tempting, but my share of just the myomectomy is probably going to be enough to break my bank.
In the meantime, when he pressed on Ignatius, I told him that I could feel it in my bladder, which needed relief already.
The more I look at the MRI image, the more I am convinced that Ignatius is not only compressing my bladder, but my spine and nerves as well, causing lower backache and occasional searing leg pains and numbness. I will soon find out.
I’ve scheduled the surgery and the pre-operative appointments (one at 7:30 a.m. on my birthday!) and received instructions. Recovery from the myomectomy seems easier and less complicated than recovery from the UFE. Dr. M. didn’t give me a definitive amount of time I’d need off (two weeks for the UFE), an there seems to be only one prescription (narcotic) painkiller and ibuprofen recommended, compared to the four prescription painkillers, antibiotics, and anti-inflammatory medications plus two nonprescription stool softeners for the UFE. I was told not to lift anything greater than 10 pounds after the UFE (Hodge fits into that category, which is part of why he took an extended vacation), but I see that I am “encouraged” not only to walk and engage in moderate exercise, but to lift up to 25 pounds. (Still, Hodge is due for another extended vacation, I think. Nothing like being chased by a fanged beast when you’re recovering from surgery.)
This time, I feel less hesitant about the necessity. I’m used to how I feel, but as Dr. T. said, “That can’t feel very good.” It’s like being 16 weeks pregnant — but for years. I want to walk without aching — and without having to be within earshot of civilization and plumbing. The 24 to 36 hours after the UFE were relentlessly painful, but I can look forward to that again if it means getting 95 percent (Dr. M.’s estimate of what he can do in this case, vs. 99 percent) of the invader’s mass off my innards and spine. It’s getting on my nerves. Literally.
Imagine — all this time, trouble, and expense began as a single muscle cell run amok.
Thirty-seven days and counting.
Addendum: J.’s reaction to the image: Is it the huge thing that reminds me of a steak because of the large white thing at the bottom (makes me think of fat on a steak)? [Note: The large white thing is my uterus.]

Before you head off for surgery, it’s good to do one or more of teh following: Have the house cleaned professionally by some yob or the other (you can always get your friends together and tell them you need these things and they should do them for you); Cook enough freezable food to last you for about 1 month, and freeze it – hearty stews and soups are best, cos you won’t feel like cooking for a bit; and see if you can get close friends and relatives to visit regularly on a schedule (like, right around when you have to take your meds. Best of luck, and death to Iggie!
Now that I’ve seen the Igster, it’s time to bid him bye bye. He does look freakishly steakish.
Erin
Embolized fibroid: Dead muscle tissue.
Steak: Dead muscle tissue.
Hmmm.
Hmmm, and I have my annual wellness exam 37 days from the date of this post.
Good luck!
Hi Diane,
I have been following Ignatius’ escapade with interest because I, too, have fibroids. Are there any new developments, details, or tidbits? What happened at your pre-op appt.? Are you looking forward to getting it over? I suspect you are simply taking it easy, trying to relax and be in the right frame of mind for your surgery and skipping blogging for the time being.
Good luck to you, Diane, and to Dr. M., too. May God bless you with a successful surgery and a good health outcome.